 |
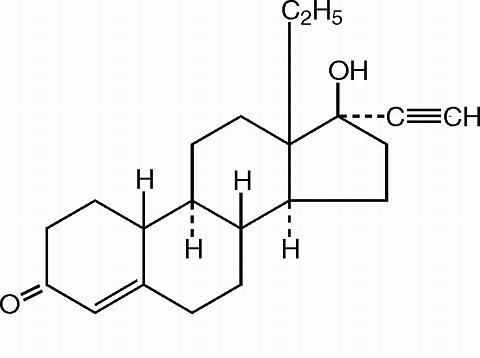
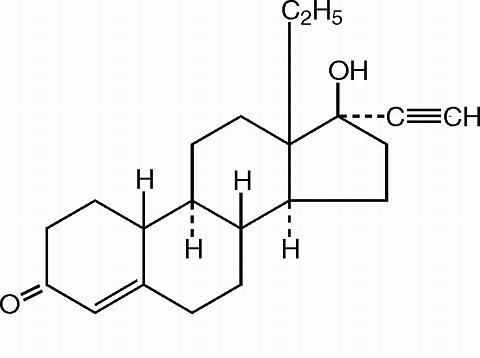
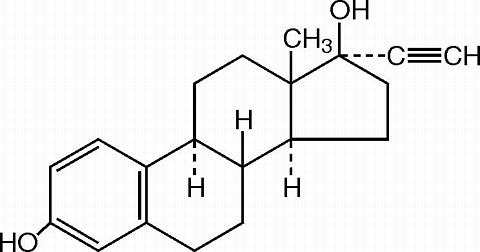
21 pink active tablets each containing 0.10 mg of levonorgestrel, d(-)-13(beta)-ethyl-17(alpha)-ethinyl-17(beta)-hydroxygon- 4-en-3-one, a totally synthetic progestogen, and 0.02 mg of ethinyl estradiol, 17(alpha)-ethinyl-1,3,5(10)-estratriene-3, 17(beta)-diol. The inactive ingredients present are cellulose, hydroxypropyl methylcellulose, iron oxide, lactose, magnesium stearate, polacrilin potassium, polyethylene glycol, titanium dioxide, and wax E.
 |
Levonorgestrel
 |
Combination oral contraceptives act by suppression of gonadotropins. Although the primary mechanism of this action is inhibition of ovulation, other alterations include changes in the cervical mucus (which increase the difficulty of sperm entry into the uterus) and the endometrium (which reduce the likelihood of implantation).
No specific investigation of the absolute bioavailability of Alesse in humans has been conducted. However, literature indicates that levonorgestrel is rapidly and completely absorbed after oral administration (bioavailability about 100%) and is not subject to first-pass metabolism. Ethinyl estradiol is rapidly and almost completely absorbed from the gastrointestinal tract but, due to first-pass metabolism in gut mucosa and liver, the bioavailability of ethinyl estradiol is between 38% and 48%.
After a single dose of Alesse to 22 women under fasting conditions, maximum serum concentrations of levonorgestrel are 2.8 ± 0.9 ng/mL (mean ± SD) at 1.6 ± 0.9 hours. At steady state, attained from day 19 onwards, maximum levonorgestrel concentrations of 6.0 ± 2.7 ng/mL are reached at 1.5 ± 0.5 hours after the daily dose. The minimum serum levels of levonorgestrel at steady state are 1.9 ± 1.0 ng/mL. Observed levonorgestrel concentrations increased from day 1 (single dose) to days 6 and 21 (multiple doses) by 34% and 96%, respectively (Figure 1). Unbound levonorgestrel concentrations increased from day 1 to days 6 and 21 by 25% and 83%, respectively. The kinetics of total levonorgestrel are non-linear due to an increase in binding of levonorgestrel to sex hormone binding globulin (SHBG), which is attributed to increased SHBG levels that are induced by the daily administration of ethinyl estradiol.
Following a single dose, maximum serum concentrations of ethinyl estradiol of 62 ± 21 pg/mL are reached at 1.5 ± 0.5 hours. At steady state, attained from at least day 6 onwards, maximum concentrations of ethinyl estradiol were 77 ± 30 pg/mL and were reached at 1.3 ± 0.7 hours after the daily dose. The minimum serum levels of ethinyl estradiol at steady state are 10.5 ± 5.1 pg/mL. Ethinyl estradiol concentrations did not increase from days 1 to 6, but did increase by 19% from days 1 to 21 (Figure 1).
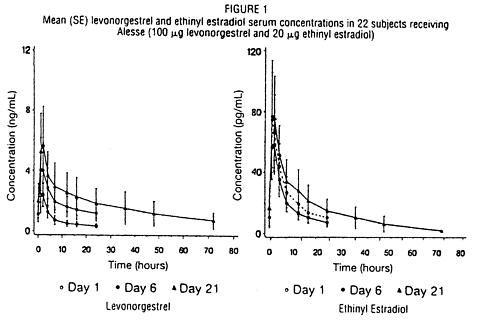 |
Table I provides a summary of levonorgestrel and ethinyl estradiol pharmacokinetic parameters.
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Levonorgestrel in serum is primarily bound to SHBG. Ethinyl estradiol is about 97% bound to plasma albumin. Ethinyl estradiol does not bind to SHBG, but induces SHBG synthesis.
Metabolism
Levonorgestrel: The most important metabolic pathway occurs in the reduction of the (DELTA)4-3-oxo group and hydroxylation at positions 2(alpha), 1(beta), and 16(beta), followed by conjugation. Most of the metabolites that circulate in the blood are sulfates of 3(alpha),5(beta)-tetrahydro-levonorgestrel, while excretion occurs predominantly in the form of glucuronides. Some of the parent levonorgestrel also circulates as 17(beta)-sulfate. Metabolic clearance rates may differ among individuals by several-fold, and this may account in part for the wide variation observed in levonorgestrel concentrations among users.
Ethinyl estradiol: Cytochrom P450 enzymes (CYP3A4) in the liver are responsible for the 2-hydroxylation that is the major oxidative reaction. The 2-hydroxy metabolite is further transformed by methylation and glucuronidation prior to urinary and fecal excretion. Levels of Cytochrome P450 (CYP3A) vary widely among individuals and can explain the variation in rates of ethinyl estradiol 2-hydroxylation. Ethinyl estradiol is excreted in the urine and feces as glucuronide and sulfate conjugates, and undergoes enterohepatic circulation.
Excretion
The elimination half-life for levonorgestrel is approximately 36 ± 13 hours at steady state. Levonorgestrel and its metabolites are primarily excreted in the urine (40% to 68%) and about 16% to 48% are excreted in feces. The elimination half-life of ethinyl estradiol is 18 ± 4.7 hours at steady state.
Race
Based on the pharmacokinetic study with Alesse, there are no apparent differences in pharmacokinetic parameters among women of different races.
No formal studies have evaluated the effect of hepatic disease on the disposition of Alesse. However, steroid hormones may be poorly metabolized in patients with impaired liver function.
No formal studies have evaluated the effect of renal disease on the disposition of Alesse.
Interactions between ethinyl estradiol and other drugs have been reported in the literature.
Oral contraceptives are indicated for the prevention of pregnancy in women who elect to use this product as a method of contraception.
Oral contraceptives are highly effective. Table II lists the typical accidental pregnancy rates for users of combination oral contraceptives and other methods of contraception. The efficacy of these contraceptive methods, except sterilization, the IUD, and Norplant® System, depends upon the reliability with which they are used. Correct and consistent use of methods can result in lower failure rates.
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
In a clinical trial with Alesse, 1,477 subjects had 7,720 cycles of use and a total of 5 pregnancies were reported. This represents an overall pregnancy rate of 0.84 per 100 woman-years. This rate includes patients who did not take the drug correctly. One or more pills were missed during 1,479 (18.8%) of the 7,870 cycles; thus all tablets were taken during 6,391 (81.2%) of the 7,870 cycles. Of the total 7,870 cycles, a total of 150 cycles were excluded from the calculation of the Pearl index due to the use of backup contraception and/or missing 3 or more consecutive pills.
Oral contraceptives should not be used in women with any of the following conditions:
Thrombophlebitis or thromboembolic disorders
A past history of deep-vein thrombophlebitis or thromboembolic disorders
Cerebrovascular or coronary artery disease
Known or suspected carcinoma of the breast
Carcinoma of the endometrium or other known or suspected estrogen-dependent neoplasia
Undiagnosed abnormal genital bleeding
Cholestatic jaundice of pregnancy or jaundice with prior pill use
Hepatic adenomas or carcinomas
Known or suspected pregnancy
| Cigarette smoking increases the risk of serious cardiovascular side effects from oral-contraceptive use. This risk increases with age and with heavy smoking (15 or more cigarettes per day) and is quite marked in women over 35 years of age. Women who use oral contraceptives should be strongly advised not to smoke. |
The use of oral contraceptives is associated with increased risks of several serious conditions including myocardial infarction, thromboembolism, stroke, hepatic neoplasia, gallbladder disease, and hypertension, although the risk of serious morbidity or mortality is very small in healthy women without underlying risk factors. The risk of morbidity and mortality increases significantly in the presence of other underlying risk factors such as certain inherited thrombophilias, hypertension, hyperlipidemias, obesity and diabetes.
Practitioners prescribing oral contraceptives should be familiar with the following information relating to these risks.
The information contained in this package insert is principally based on studies carried out in patients who used oral contraceptives with higher formulations of estrogens and progestogens than those in common use today. The effect of long-term use of the oral contraceptives with lower doses of both estrogens and progestogens remains to be determined.
Throughout this labeling, epidemiological studies reported are of two types: retrospective or case control studies and prospective or cohort studies. Case control studies provide a measure of the relative risk of disease, namely, a ratio of the incidence of a disease among oral-contraceptive users to that among nonusers. The relative risk does not provide information on the actual clinical occurrence of a disease. Cohort studies provide a measure of attributable risk, which is the difference in the incidence of disease between oral-contraceptive users and nonusers. The attributable risk does provide information about the actual occurrence of a disease in the population. For further information, the reader is referred to a text on epidemiological methods.
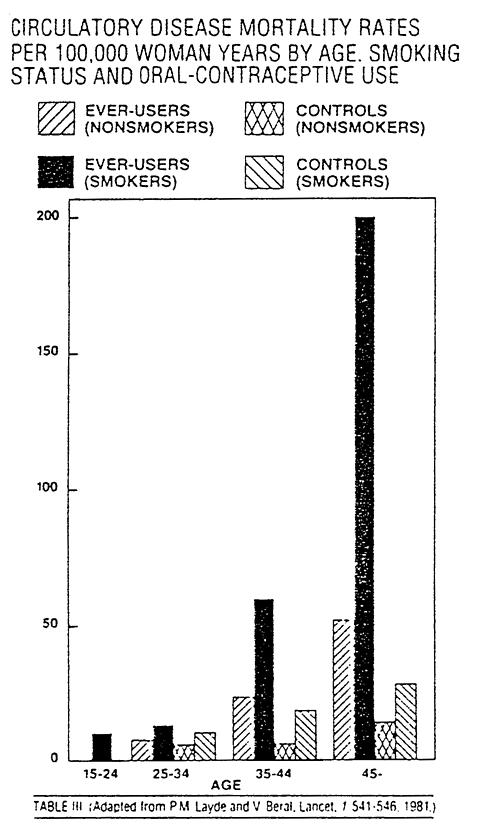 |
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Patients should be counseled that this product does not protect against HIV infection (AIDS) and other sexually transmitted diseases.
1. PHYSICAL EXAMINATION AND FOLLOW-UP
A periodic history and physical examination is appropriate for all women, including women using oral contraceptives. The physical examination, however, may be deferred until after initiation of oral contraceptives if requested by the woman and judged appropriate by the clinician. The physical examination should include special reference to blood pressure, breasts, abdomen and pelvic organs, including cervical cytology, and relevant laboratory tests. In case of undiagnosed, persistent or recurrent abnormal vaginal bleeding, appropriate diagnostic measures should be conducted to rule out malignancy. Women with a strong family history of breast cancer or who have breast nodules should be monitored with particular care.
2. LIPID DISORDERS
Women who are being treated for hyperlipidemias should be followed closely if they elect to use oral contraceptives. Some progestogens may elevate LDL levels and may render the control of hyperlipidemias more difficult. (See " Warnings " , 1d.)
In patients with familial defects of lipoprotein metabolism receiving estrogen-containing preparations, there have been case reports of significant elevations of plasma triglycerides leading to pancreatitis.
If jaundice develops in any woman receiving such drugs, the medication should be discontinued. Steroid hormones may be poorly metabolized in patients with impaired liver function.
Oral contraceptives may cause some degree of fluid retention. They should be prescribed with caution, and only with careful monitoring, in patients with conditions which might be aggravated by fluid retention.
5. EMOTIONAL DISORDERS
Patients becoming significantly depressed while taking oral contraceptives should stop the medication and use an alternative method of contraception in an attempt to determine whether the symptom is drug related. Women with a history of depression should be carefully observed and the drug discontinued if depression recurs to a serious degree.
6. CONTACT LENSES
Contact-lens wearers who develop visual changes or changes in lens tolerance should be assessed by an ophthalmologist.
7. DRUG INTERACTIONS
Reduced efficacy and increased incidence of breakthrough bleeding and menstrual irregularities have been associated with concomitant use of rifampin. A similar association, though less marked, has been suggested with barbiturates, phenylbutazone, phenytoin, and possibly with griseofulvin, ampicillin, and tetracyclines.
Troleadomycin may increase the risk of intrahepatic cholestasis during coadministration with combination oral contraceptives.
8. INTERACTIONS WITH LABORATORY TESTS
Certain endocrine- and liver-function tests and blood components may be affected by oral contraceptives:
a. Increased prothrombin and factors VII, VIII, IX, and X; decreased antithrombin 3; increased norepinephrine-induced platelet aggregability.
b. Increased thyroid-binding globulin (TBG) leading to increased circulating total thyroid hormone, as measured by protein-bound iodine (PBI), T4 by column or by radioimmunoassay. Free T3 resin uptake is decreased, reflecting the elevated TBG; free T4 concentration is unaltered.
c. Other binding proteins may be elevated in serum.
d. Sex-hormone binding globulins are increased and result in elevated levels of total circulating sex steroids; however, free or biologically active levels remain unchanged.
e. Triglycerides may be increased.
f. Glucose tolerance may be decreased.
g. Serum folate levels may be depressed by oral-contraceptive therapy. This may be of clinical significance if a woman becomes pregnant shortly after discontinuing oral contraceptives.
10. PREGNANCY
Pregnancy Category X. See " Contraindications " and " Warnings " sections.
11. NURSING MOTHERS
Small amounts of oral-contraceptive steroids have been identified in the milk of nursing mothers, and a few adverse effects on the child have been reported, including jaundice and breast enlargement. In addition, oral contraceptives given in the postpartum period may interfere with lactation by decreasing the quantity and quality of breast milk. If possible, the nursing mother should be advised not to use oral contraceptives but to use other forms of contraception until she has completely weaned her child.
INFORMATION FOR THE PATIENT
See Patient Labeling Printed Below.
12. PEDIATRIC USE
Safety and efficacy of Alesse have been established in women of reproductive age. Safety and efficacy are expected to be the same for postpubertal adolescents under the age of 16 and users 16 and older. Use of this product before menarche is not indicated.
An increased risk of the following serious adverse reactions has been associated with the use of oral contraceptives (see " Warnings " section):
Hypertension
Hepatic adenomas or benign liver tumors
There is evidence of an association between the following conditions and the use of oral contraceptives, although additional confirmatory studies are needed:
The following adverse reactions have been reported in patients receiving oral contraceptives and are believed to be drug related:
Vomiting
Gastrointestinal symptoms (such as abdominal cramps and bloating)
Spotting
Amenorrhea
Temporary infertility after discontinuation of treatment
Edema
Melasma which may persist
Breast changes: tenderness, enlargement, secretion
Change in weight (increase or decrease)
Change in cervical erosion and secretion
Diminution in lactation when given immediately postpartum
Migraine
Rash (allergic)
Reduced tolerance to carbohydrates
Change in corneal curvature (steepening)
Intolerance to contact lenses
The following adverse reactions have been reported in users of oral contraceptives and the association has been neither confirmed nor refuted:
Cataracts
Changes in appetite
Headache
Dizziness
Erythema multiforme
Erythema nodosum
Vaginitis
Acne
Changes in libido
Colitis
Serious ill effects have not been reported following acute ingestion of large doses of oral contraceptives by young children. Overdosage may cause nausea, and withdrawal bleeding may occur in females.
The following noncontraceptive health benefits related to the use of oral contraceptives are supported by epidemiological studies which largely utilized oral-contraceptive formulations containing doses exceeding 0.035 mg of ethinyl estradiol or 0.05 mg of mestranol.
Effects on menses:
Increased menstrual cycle regularity
Decreased blood loss and decreased incidence of iron-deficiency anemia
Decreased incidence of dysmenorrhea
Effects related to inhibition of ovulation:
Decreased incidence of functional ovarian cysts
Decreased incidence of ectopic pregnancies
Effects from long-term use:
Decreased incidence of fibroadenomas and fibrocystic disease of the breast
Decreased incidence of acute pelvic inflammatory disease
Decreased incidence of endometrial cancer
Decreased incidence of ovarian cancer
To achieve maximum contraceptive effectiveness, Alesse™ must be taken exactly as directed and at intervals not exceeding 24 hours. The dispenser should be kept in the wallet supplied to avoid possible fading of the pills. If the pills fade, patients should continue to take them as directed.
The dosage of Alesse-21 is one pink tablet daily for 21 consecutive days, followed by 7 days when no tablets are taken.
It is recommended that Alesse-21 tablets be taken at the same time each day.
Sunday start:
During the first cycle of medication, the patient is instructed to begin taking Alesse-21 on the first Sunday after the onset of menstruation. If menstruation begins on a Sunday, the first tablet (pink) is taken that day. One pink tablet should be taken daily for 21 consecutive days, followed by seven days when no tablet is taken. Withdrawal bleeding should usually occur within three days following discontinuation of pink tablets. During the first cycle, contraceptive reliance should not be placed on Alesse-21 until a pink tablet has been taken daily for 7 consecutive days. The possibility of ovulation and conception prior to initiation of medication should be considered.
The patient begins her next and all subsequent 21-day courses of tablets on the same day of the week (Sunday) on which she began her first course, following the same schedule: 21 days on pink tablets--7 days when no tablets are taken. If in any cycle the patient starts tablets later than the proper day, she should protect herself against pregnancy by using another method of birth control until she has taken a pink tablet daily for 7 consecutive days.
Day 1 start:
During the first cycle of medication, the patient is instructed to begin taking Alesse-21 during the first 24 hours of her period (day one of her menstrual cycle). One pink tablet should be taken daily for 21 consecutive days. Withdrawal bleeding should usually occur within three days following discontinuation of pink tablets. If medication is begun on day one of the menstrual cycle, no back-up contraception is necessary. If Alesse-21 tablets are started later than day one of the first menstrual cycle or postpartum, contraceptive reliance should not be placed on Alesse-21 tablets until after the first 7 consecutive days of administration. The possibility of ovulation and conception prior to initiation of medication should be considered.
When the patient is switching from a 21-day regimen of tablets, she should wait 7 days after her last tablet before she starts Alesse. She will probably experience withdrawal bleeding during that week. She should be sure that no more than 7 days pass after her previous 21-day regimen. When the patient is switching from a 28-day regimen of tablets, she should start her first pack of Alesse on the day after her last tablet. She should not wait any days between packs.
If spotting or breakthrough bleeding occur, the patient is instructed to continue on the same regimen. This type of bleeding is usually transient and without significance; however, if the bleeding is persistent or prolonged, the patient is advised to consult her physician. While there is little likelihood of ovulation occurring if only one or two pink tablets are missed, the possibility of ovulation increases with each successive day that scheduled pink tablets are missed. Although the occurrence of pregnancy is unlikely if Alesse is taken according to directions, if withdrawal bleeding does not occur, the possibility of pregnancy must be considered. If the patient has not adhered to the prescribed schedule (missed one or more tablets or started taking them on a day later than she should have), the probability of pregnancy should be considered at the time of the first missed period and appropriate diagnostic measures taken before the medication is resumed. If the patient has adhered to the prescribed regimen and misses two consecutive periods, pregnancy should be ruled out before continuing the contraceptive regimen.
The risk of pregnancy increases with each active (pink) tablet missed. For additional patient instructions regarding missed tablets, see the " WHAT TO DO IF YOU MISS PILLS " section in the DETAILED PATIENT LABELING below.
In the nonlactating mother, Alesse may be initiated postpartum, for contraception. When the tablets are administered in the postpartum period, the increased risk of thromboembolic disease associated with the postpartum period must be considered (See " Contraindications ", " Warnings ", and " Precautions " concerning thromboembolic disease).
Alesse™-21 tablets (0.10 mg levonorgestrel and 0.02 mg ethinyl estradiol) are available in packages of 3 MINI-PACK™ dispensers of 21 tablets each, NDC 0008-0912-02, as follows:
21 active tablets. NDC 0008-0912, pink, round tablet marked "" and "912".
Store at controlled room temperature 20°-25° C (68°-77° F).
References available upon request.
 |
This product (like all oral contraceptives) is intended to prevent pregnancy. It does not protect against HIV infection (AIDS) and other sexually transmitted diseases.
Oral contraceptives, also known as "birth-control pills" or "the pill", are taken to prevent pregnancy, and when taken correctly, have a failure rate of less than 1.0% per year when used without missing any pills. The typical failure rate of large numbers of pill users is less than 3.0% per year when women who miss pills are included. For most women oral contraceptives are also free of serious or unpleasant side effects. However, forgetting to take pills considerably increases the chances of pregnancy.
For the majority of women, oral contraceptives can be taken safely. But there are some women who are at high risk of developing certain serious diseases that can be life-threatening or may cause temporary or permanent disability or death. The risks associated with taking oral contraceptives increase significantly if you:
You should not take the pill if you suspect you are pregnant or have unexplained vaginal bleeding.
| Cigarette smoking increases the risk of serious adverse effects on the heart and blood vessels from oral-contraceptive use. This risk increases with age and with heavy smoking (15 or more cigarettes per day) and is quite marked in women over 35 years of age. Women who use oral contraceptives should not smoke. |
Most side effects of the pill are not serious. The most common such effects are nausea, vomiting, bleeding between menstrual periods, weight gain, breast tenderness, and difficulty wearing contact lenses. These side effects, especially nausea and vomiting, may subside within the first three months of use.
The serious side effects of the pill occur very infrequently, especially if you are in good health and do not smoke. However, you should know that the following medical conditions have been associated with or made worse by the pill:
The symptoms associated with these serious side effects are discussed in the detailed leaflet given to you with your supply of pills. Notify your doctor or health-care provider if you notice any unusual physical disturbances while taking the pill. In addition, drugs such as rifampin, as well as some anticonvulsants and some antibiotics, may decrease oral-contraceptive effectiveness.
Breast cancer has been diagnosed slightly more often in women who use the pill than in women of the same age who do not use the pill. This very small increase in the number of breast cancer diagnoses gradually disappears during the 10 years after stopping use of the pill. It is not known whether the difference is caused by the pill. It maybe that women taking the pill were examined more often, so that breast cancer was more likely to be detected.
Some studies have found an increase in the incidence of cancer or precancerous lesions of the cervix in women who use the pill. However, this finding may be related to factors other than the use of the pill.
Taking the pill provides some important noncontraceptive benefits. These include less painful menstruation, less menstrual blood loss and anemia, fewer pelvic infections, and fewer cancers of the ovary and the lining of the uterus.
Be sure to discuss any medical condition you may have with your health-care provider. Your health-care provider will take a medical and family history before prescribing oral contraceptives and will examine you. The physical examination may be delayed to another time if you request it and the health-care provider believes that it is appropriate to postpone it. You should be reexamined at least once a year while taking oral contraceptives. The detailed patient information leaflet gives you further information which you should read and discuss with your health-care provider.
This product (like all oral contraceptives) is intended to prevent pregnancy. It does not protect against transmission of HIV (AIDS) and other sexually transmitted diseases such as chlamydia, genital herpes, genital warts, gonorrhea, hepatitis B, and syphilis.
This product (like all oral contraceptives) is intended to prevent pregnancy. It does not protect against HIV infection (AIDS) and other sexually transmitted diseases.
INTRODUCTION
Any woman who considers using oral contraceptives (the birth-control pill or the pill) should understand the benefits and risks of using this form of birth control. This leaflet will give you much of the information you will need to make this decision and will also help you determine if you are at risk of developing any of the serious side effects of the pill. It will tell you how to use the pill properly so that it will be as effective as possible.
However, this leaflet is not a replacement for a careful discussion between you and your health-care provider. You should discuss the information provided in this leaflet with him or her, both when you first start taking the pill and during your revisits. You should also follow your health-care provider's advice with regard to regular check-ups while you are on the pill.
EFFECTIVENESS OF ORAL CONTRACEPTIVES
Oral contraceptives or "birth-control pills" or "the pill" are used to prevent pregnancy and are more effective than other nonsurgical methods of birth control. When they are taken correctly, the chance of becoming pregnant is less than 1.0% per year when used perfectly, without missing any pills.
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
WHO SHOULD NOT TAKE ORAL CONTRACEPTIVES
| Cigarette smoking increases the risk of serious adverse effects on the heart and blood vessels from oral-contraceptive use. This risk increases with age and with heavy smoking (15 or more cigarettes per day) and is quite marked in women over 35 years of age. Women who use oral contraceptives should not smoke. |
Some women should not use the pill. For example, you should not take the pill if you are pregnant or think you may be pregnant. You should also not use the pill if you have had any of the following conditions:
Or, if you have any of the following:
Tell your health-care provider if you have ever had any of these conditions. Your health-care provider can recommend another method of birth control.
OTHER CONSIDERATIONS BEFORE TAKING ORAL CONTRACEPTIVES
Tell your health-care provider if you or any family member has ever had:
Women with any of these conditions should be checked often by their health-care provider if they choose to use oral contraceptives. Also, be sure to inform your doctor or health-care provider if you smoke or are on any medications.
RISKS OF TAKING ORAL CONTRACEPTIVES
Breast cancer has been diagnosed slightly more often in women who use the pill than in women who do not use the pill. This very small increase in the number of breast cancer diagnoses gradually disappears after stopping the use of the pill. It is not known whether the difference is caused by the pill. It may be that women taking the pill were examined more often, so that breast cancer was more likely to be detected.
Some studies have found an increase in the incidence of cancer or precancerous lesions of the cervix in women who use oral contraceptives. However, this finding may be related to factors other than the use of oral contraceptives.
ESTIMATED RISK OF DEATH FROM A BIRTH CONTROL METHOD OR PREGNANCY
All methods of birth control and pregnancy are associated with a risk of developing certain diseases which may lead to disability or death. An estimate of the number of deaths associated with different methods of birth control and pregnancy has been calculated and is shown in the following table.
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
In the above table, the risk of death from any birth-control method is less than the risk of childbirth, except for oral-contraceptive users over the age of 35 who smoke and pill users over the age of 40 even if they do not smoke. It can be seen in the table that for women aged 15 to 39, the risk of death was highest with pregnancy (7 to 26 deaths per 100,000 women, depending on age). Among pill users who do not smoke, the risk of death was always lower than that associated with pregnancy for any age group, except for those women over the age of 40, when the risk increases to 32 deaths per 100,000 women, compared to 28 associated with pregnancy at that age. However, for pill users who smoke and are over the age of 35, the estimated number of deaths exceeds those for other methods of birth control. If a woman is over the age of 40 and smokes, her estimated risk of death is four times higher (117/100,000 women) than the estimated risk associated with pregnancy (28/100,000 women) in that age group.
The suggestion that women over 40 who don't smoke should not take oral contraceptives is based on information from older high-dose pills and on less-selective use of pills than is practiced today. An Advisory Committee of the FDA discussed this issue in 1989 and recommended that the benefits of oral-contraceptive use by healthy, nonsmoking women over 40 years of age may outweigh the possible risks. However, all women, especially older women, are cautioned to use the lowest-dose pill that is effective.
WARNING SIGNALS
If any of these adverse effects occur while you are taking oral contraceptives, call your doctor immediately:
6. Lipid metabolism and inflammation of the pancreas
In patients with inherited defects of lipid metabolism, there have been reports of significant elevations of plasma triglycerides during estrogen therapy. This has lead to pancreatitis in some cases.
SIDE EFFECTS OF ORAL CONTRACEPTIVES
Other side effects may include change in appetite, headache, nervousness, depression, dizziness, loss of scalp hair, rash, and vaginal infections.
If any of these side effects bother you, call your doctor or health-care provider.
GENERAL PRECAUTIONS
BEFORE YOU START TAKING YOUR PILLS:
ANOTHER KIND OF BIRTH CONTROL (such as condoms
 |
or foam) to use as a back-up in case you miss pills.
You have a choice of which day to start taking your first pack of pills.
Decide with your doctor or clinic which is the best day for you. Pick a time of day which will be easy to remember.
21 pills: Wait 7 days to start the next pack. You will probably have your period during that week. Be sure that no more than 7 days pass between 21-day packs.
28 pills: Start the next pack on the day after your last "reminder" pill. Do not wait any days between packs.
If you MISS 1 pink "active" pill:
If you MISS 2 pink "active" pills in a row in WEEK 1 OR WEEK 2 of your pack:
If you MISS 2 pink "active" pills in a row in THE 3rd WEEK:
If you MISS 3 OR MORE pink "active" pills in a row (during the first 3 weeks):
If you forget any of the 7 light-green "reminder" pills in Week 4:
THROW AWAY the pills you missed.
Keep taking 1 pill each day until the pack is empty.
You do not need a back-up method if you start your next pack on time.
Use a BACK-UP METHOD anytime you have sex.
KEEP TAKING ONE PILL EACH DAY until you can reach your doctor or clinic.
The incidence of pill failure resulting in pregnancy is approximately less than 1.0% if taken every day as directed, but more typical failure rates are less than 3.0%. If failure does occur, the risk to the fetus is minimal.
RISKS TO THE FETUS
If you do become pregnant while using oral contraceptives, the risk to the fetus is small, on the order of no more than one per thousand. You should, however, discuss the risks to the developing child with your doctor.
Pregnancy after stopping the pill
There may be some delay in becoming pregnant after you stop using oral contraceptives, especially if you had irregular menstrual cycles before you used oral contraceptives. It may be advisable to postpone conception until you begin menstruating regularly once you have stopped taking the pill and desire pregnancy.
There does not appear to be any increase in birth defects in newborn babies when pregnancy occurs soon after stopping the pill.
Overdosage
Serious ill effects have not been reported following ingestion of large doses of oral contraceptives by young children. Overdosage may cause nausea and withdrawal bleeding in females. In case of overdosage, contact your health-care provider or pharmacist.
Other information
Your health-care provider will take a medical and family history before prescribing oral contraceptives and will examine you. The physical examination may be delayed to another time if you request it and the health-care provider believes that it is appropriate to postpone it. You should be reexamined at least once a year. Be sure to inform your health-care provider if there is a family history of any of the conditions listed previously in this leaflet. Be sure to keep all appointments with your health-care provider, because this is a time to determine if there are early signs of side effects of oral-contraceptive use.
Do not use the drug for any condition other than the one for which it was prescribed. This drug has been prescribed specifically for you; do not give it to others who may want birth-control pills.
HEALTH BENEFITS FROM ORAL CONTRACEPTIVES
In addition to preventing pregnancy, use of oral contraceptives may provide certain benefits. They are:
If you want more information about birth-control pills, ask your doctor or pharmacist. They have a more technical leaflet called the Professional Labeling which you may wish to read.
Manufactured by:
Wyeth Laboratories
A Wyeth-Ayerst Company
Philadelphia, PA 19101
CI 4843-2 Revised April 24, 1997